The basis for our new strategy is informed by advancements in suicide prevention care, along with learning from our first phase 2017/2019. We recognised that suicide can only be preventable if the care provided is based on best evidence for preventability and organised consistently, systematically and in a reliable way. The new strategy is particularly informed by:
- Themes in service provision and clinical practice from deaths by suicide
- The successes and challenges of our key interventions during the first phase
- The latest research and best practice in suicide prevention
Our Team
During our first phase a new team was created to ensure the effective implementation of Mersey Care’s Zero Suicide goal. The scope of the team has now evolved to meet the needs of the new strategy.
The group directs, oversees and monitors suicide prevention activity across the priority areas in order to ensure a comprehensive and evidenced based suicide prevention approach for our Trust.
The work plan developed to support the delivery of our Trust Strategy is monitored by the Patient Safety group.
If you would like to find out more about our Trust suicide prevention strategy and group or would like to get involved, have any thoughts or ideas please contact safefrom.suicide@merseycare.nhs.uk
The Safe from Suicide Team operate within the Centre for Perfect Care (CfPC) and is made up of several specialists in the area of suicide prevention.
Team Membership and Accountability
-
Steve Bradbury - Deputy Director for Innovation and Improvement CfPC
-
Dr Claire Iveson - Consultant Clinical Psychologist and Clinical and Strategic Lead for Safe, Safety Planning and Zero Suicide Strategy
-
Steve Messenger - Programme support and Data lead
-
Joleen Shaw - Project Manager
-
Angela Brown - CfPC Facilitator and Safe from Suicide project support
-
Lesley Bristow - Report Builder Analyst
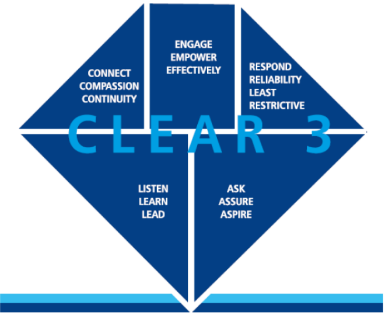 CLEAR3 is a concept, service delivery and system design model with a combination of features from research and best practice evidence deemed necessary for excellent suicide prevention care. It is a model that can be applied to all service settings and clinical systems.
CLEAR3 is a concept, service delivery and system design model with a combination of features from research and best practice evidence deemed necessary for excellent suicide prevention care. It is a model that can be applied to all service settings and clinical systems.
Transition is continually reported as a theme in our own deaths by suicide and international literature and we have no standardised protocol for enabling a “safe landing” within and out of our care. In addition research and incident learning suggests the development and inclusion of consistent effective interventions for follow up and infrequent contacts.
National policy indicates that service users who have had an in-patient stay should have a follow-up of their care within 72hrs of discharge. This is a maximum period and some service users may require additional support during initial days following discharge. Face to face contact is identified as the main process for these discharge meetings. However, alternative methods can be sort in the short term, but not as a replacement. Face-to-face meetings should be conducted at the earliest opportunity.
The latest report from the National Confidential Inquiry (NCI) indicated that from 2007 to 2017 there were 2,178 deaths by suicide within three months post discharge from hospital. 16% were within the first seven days with 21% of these occurring on the third day post discharge.
In response to this the trust has developed a process to ensure the follow-up of service users within 48hrs of discharge from an in-patient ward. The principals around this policy can be found on the attached paper. These follow the processes explained within the CLEAR3 model of care.
The Trust have made a commitment to implement an agreed transition protocol to standardise practice and quality of care for all those who move within and out of our services using a standardised approach (checklist/protocol).
The transition protocol describes the steps that should be taken as a minimum safe standard for transition. As an example, the steps below describe the discharge/transition that will be required from psychiatric inpatient care to community teams:
- Identify who will complete the follow up and where possible introduce them to the service user and as a minimum the individual should know who is visiting them at home and when.
- Steps should be taken to identify significant other and involve them in discharge planning prior to discharge.
- Have risks surrounding the provision of medicines been considered as per zero suicide policy and personal risks of overdose.
- All service users leaving hospital should have been offered a safety plan and it should be up to date. Access to lethal means and plans to mitigate should have been discussed via the safety planning intervention and with significant other. Consider the use of brief problem solving, any psychoeducation and information to help with transition. (utilise safety plan resource list)
- Has the GP been contacted to inform of discharge and their role to support individual and/ or any recommendations for ongoing care.
- Are there further referrals to be made to other therapies, services i.e. Drug and alcohol. Are there any barriers to engagement and has this been considered and trouble shooted with the service user?
- Have short term goals for treatment, and recovery been identified and actioned or transferred to follow up contact to revisit
- Has a process been identified if the person is not available for follow up contact? Is there a plan to ensure further follow up and contact is sought.
- The Transition protocol will provide a checklist for staff
- Has careful consideration been given to whether the service user requires and chooses an earlier follow up, more than one follow up and via what means this should be delivered i.e. telephone, virtual or face to face. (see below for outline of factors to consider)
As a key trust suicide prevention prirotiy, it is important that this process is built into the system of care and becomes routine practice undertaken by an allocated individual. The model is a set of practical tasks that all those trained in eRisk should be able to complete.
A RIO template has been built to support the transtion process so that staff can input information and document actions and next steps when they carry out the contact. The template will also allow inpatient staff to record important information that they wish the practitioner conducting the follow up to review. This should sit under risk information alongside the “my safety plan” record. The quality of the follow ups once implemented and embedded into Business as Usual will be subject to audit for quality compliance.
The transtion process as described above (and associated RIO documentation) is due to be tested in the next 6 to 12 months.
The adoption of a 5Question approach will be utilised in some areas where contact is consistent but over longer periods of time. These questions will focus upon checking the service users current risks and support. Questions being
- General wellbeing and circumstances
- Asking how they are and has anything changed since the last contact, such as financial/housing problems, mood, current daily living
- Exploring risks
- Do verbal and non-verbal responses match or has any new risk been identified based on current circumstances
- Significant other support
- Are there people to support them during daily living. Are the contact details for these people correct should we need to contact them.
- Problem solving
- Look at ways any problems highlighted may be solved, including updating safety plans.
- Immediate Actions
- What or who needs to do a particular action to maintain safety for any risks identified.
eRisk (effective Risk Intervention SKills) training aims to enhance knowledge, skills, competencies, and confidence of the workforce to carry out risk assessments, formulation, management plans and safety plans. The eRISK training will give you basic information into the development of a Risk Assessment and how to formulate this risk to develop management plans and safety plans.
Please see training section for more information
Our data shows that service users that are ‘high risk’ have contact with A&E, triage car and multiple DNAs additionally those with substance misuse have a significantly statistically higher risk of completing suicide. This is consistent with national and international evidence and our internal suicide prevention strategy.
The trust is looking at alternative ways to support staff in these areas to provide safe and effective care to our service users we only see for brief periods of time through the year.
Some service users will be offered a brief interventions safety flashcard to support them during increased periods of risk. This can be further developed if they require increased support from CMHT or In-patient settings.
Additional compassionate support will be offered by means of a follow-up text message to the service user after contact with services. This will check they are still safe and direct to specific contact numbers or on the trust's ‘we care’ support page.
Useful documents
The trust aims to reduce ligature use through our ligature reduction action plan across inpatient services, to reduce the distress such incidents can have on all those involved. The ligature reduction action plan includes therapeutic interventions, trauma-informed care, self-harm interventions, safety plans, least restrictive practice, risk management, transitions in care, and operational issues. The action plan is based on the recommendations within the Ligature Reduction Guide
A recent review of our data indicated that over 40% of people who went on to take their own life had underlying physical health conditions. Specific conditions included heart, respiratory and chronic pain and staff do not currently have training available beyond an awareness level.
Work is ongoing, with physical health teams, to develop on training programmes that have been delivered to specialist teams work with specific chronic physical health conditions.
Further information of these developments will be available in due course.
We know that approaches to prevention must be wide-ranging and addressed across the system. For this reason, we have worked to ensure our strategy aligns with the wider regional strategies in Cheshire and Merseyside. We work alongside our system partners as part of the council led local suicide prevention groups to monitor progress and share learning to inform future action planning.
We recognise that it’s the responsibility of all partners to work together to prevent suicide.